Bouncing back ain’t what it used to be
Has it been taking you longer to recover lately, from…literally everything? In the past few years, a lot more of us have used up our bandwidth, yet we expect to be able to “push through” in the same way we used to. It may be that the pushing through itself was always bad for us, but we didn’t feel the effects until we used up everything we had. We hear a lot about resilience, but the fact is, we live in a culture that glorifies crunch and encourages pushing through to the detriment of physical and mental health, and it’s killing us. While there are certainly ways to increase resilience, we are finite. There are already enough external things killing us; we need to stop the self-destruction and learn to treat ourselves sustainably.
What does “pushing through” mean?
“Pushing through” is forcing yourself to function past your physical or emotional limits, past capacity: Staying up all night to finish a task. Working week after week without a day off until you feel numb. Exercising until you throw up. Prioritizing others’ feelings and keeping silent when your own heart is breaking. Ignoring hunger, thirst, or the need to go to the bathroom for just another hour and then another hour. Staying in an intolerable situation and telling yourself you “should” just be able to tolerate it. Often needing caffeine, aspirin, or alcohol to tolerate the situation. Do any of those sound familiar?
Consequences of pushing through
Here’s the thing. Any time you push through your limits–physical or emotional–you are borrowing from your future self. You are eating your seed corn. You are going in debt to your own physical and mental health. You are spending resources you don’t have! The discomfort is there for a reason. It tells you when you have reached your limit, when to stop spending yourself, when you are tapped out and used up. The discomfort is the sign to stop.
When people say “listen to your body,” what that means is if it hurts, stop doing it. If you are tired, rest. If you are sad, cry. If you are hungry, eat. This sounds simplistic, but many of us have been conditioned since childhood to ignore or “push through” our limits. We may have a high tolerance for physical and emotional discomfort. Well, guess what? That’s often harmful. It may be lifesaving in a situation of desperate crisis, but it’s not sustainable. You can tolerate the situations causing the discomfort for the short term, but you are spending yourself to do so. You are spending your future self for today’s emergency. Burning out is the direct result of pushing through too many times. It means the future self you spent is today’s self.
Why do we overspend ourselves?
Many of us have been taught that we are expendable, and that discomfort is always something to be ignored as we push through it to a goal. We learn that spending ourselves recklessly is okay or even admirable as long as it’s in service of a worthy goal. Sometimes it’s a goal we want to reach, but often it’s a goal others have set for us, a social expectation, a “should.”
You may be fighting to not feel your reactions to a given situation, when what really needs to happen is for you to leave or change the situation. The reactions you’re experiencing are an important indicator of how the situation is affecting you, rather than a distraction to be ignored or suppressed.
Learning to respect your own limits
Before you can set limits, you need to know what your limits are. When you push through, what is it you are pushing through? Is it exhaustion? Fatigue is a sign you need to rest. Pain? Pain is a sign that something may be injuring you. Is it fear? Fear is a sign that something may hurt you. Is it resentment? Resentment is a sign that you are giving more than you can afford to give. These are important indicators of how you are being affected.
What if you don’t know your limits? In particular, survivors of abuse or neglect are vulnerable to not having well-developed boundaries, that is: knowing your limits. That’s because in an important part of your development, you were taught that how you felt about things was not important. You were not allowed to develop boundaries or learn your limits, so you developed a high tolerance for discomfort. Too high, in fact! As a result, what often happens is you don’t realize that your limits have been reached until they are surpassed, and then you are utterly overwhelmed.
Therefore, your task in adulthood is to lower your tolerance for discomfort. We want you to learn to stop what you’re doing before the discomfort gets to the point of overwhelm, by reducing your threshold of tolerance for discomfort. Notice which feelings indicate things are too much for you. (Exhaustion? Pain? Fear? Resentment?) The goal is to start noticing and paying actual attention to discomforts when they are still small, taking them seriously while they are still small. Initially this will feel selfish or silly or spoiled. You will feel guilty! But in fact it is solid progress.
Does this mean we should strive to never feel discomfort? Of course not. Discomfort is an integral part of being human, part of progressing, part of growing and living with others. But we can learn to discern between the discomfort of healthy growth, and discomfort that is an indicator that we aren’t taking care of ourselves or are actively being harmed. There is no need to valorize discomfort for the sake of discomfort.
Is it ever okay to push through?
There are exceptions where it’s okay to intentionally, consciously push your limits or overspend yourself. Maybe you’re doing physical therapy to recover from a surgery and the exercises hurt. This is for a very specific recovery goal and it’s under the supervision of an expert; the point is not to just do something very hard that hurts, it’s to heal. Or maybe you have a phobia and you know a particular fear is irrational and you want to overcome it. But again, this is a very specific exception and you can engage carefully knowing that you’re actually safe; the point is not to just ignore fear.
Maybe you intentionally incur short-term temporary debts to your future self: you occasionally stay up to finish a paper or meet a work deadline, you’re training for a special sports event that you enjoy, you’re taking care of a loved one who is ill. In those cases you support your well-being, you plan how to “pay it back” to yourself immediately by taking a few days to catch up on sleep, do stretches, feed yourself well, socialize, do your journaling, relax. Then you’ve repaid yourself and repaired your body and emotions. And in each case, these are goals that you have chosen because you value them yourself.
But all too often, what we’re doing is not one of these exceptions. Instead, we’re relying on emergency spending as a way of life. We are pushing through important warnings to stop!
Spend yourself less and pay yourself back more
Learn your limits. What tires you out? What hurts physically? What interactions leave you emotionally derailed or spent? There was a point where the discomfort began–did you notice it then, or not until it became overwhelming?
Choose your goals. Spend yourself intentionally on the things that really matter to you, instead of habitually overspending yourself on things that don’t help you survive or make you happy.
Respect your limits. Stop doing the things that always lead to those feelings! Either stop doing them entirely, or stop doing them while the discomfort is still mild. Stop when you only feel a little tired, not when you’re already exhausted. Or stop when you’re just a little sore, not when you can’t stand because you overworked your muscles. Or end a phone conversation when you’re only a little antsy, instead of staying on the line until you feel resentful.
Pay yourself back. This sounds so simple, yet it’s not easy. Rest, eat, comfort and entertain yourself after spending yourself. Restore yourself! You cannot simply jump back into routine without restoring whatever you have overspent, or you’ll be running at a deficit. Do not allow a self-care deficit to become chronic–that leads to illness.
What if I just can’t
In some cases, there are times we know we are beyond capacity, but we are running ourselves ragged just to make ends meet or keep our lives holding together. This unfortunately and unfairly contributes to illness and even shorter lifespan for those in marginalized groups: racialized groups, those who are poor, and disabled people, for example.
In that situation, I encourage you to let go of tasks that are not an absolute necessity. Do what you must and do what you want, but let go of doing what you “should.” By this I mean, prioritize the tasks that will get your bills paid, and prioritize the things that will help you stay functioning (make you happy or relax you). However, let go of things you’re doing because it’s a “should” instead of a need or a want. De-prioritize things that you’re mainly doing because of the judgments, habits, or opinions of others.
You are a finite resource
A big part of increasing resilience is learning what our limits are and respecting them, instead of pushing through them. Learn to stop when discomfort is small, not after it becomes overwhelming. Some goals may be worth temporarily overspending ourselves, but we must choose those goals carefully and with intention, and then make sure to pay ourselves back. Do not let a deficit become chronic: you are borrowing from your future self. Stop pushing through the warnings. You are a finite resource. You are irreplaceable.
Become sustainable. 
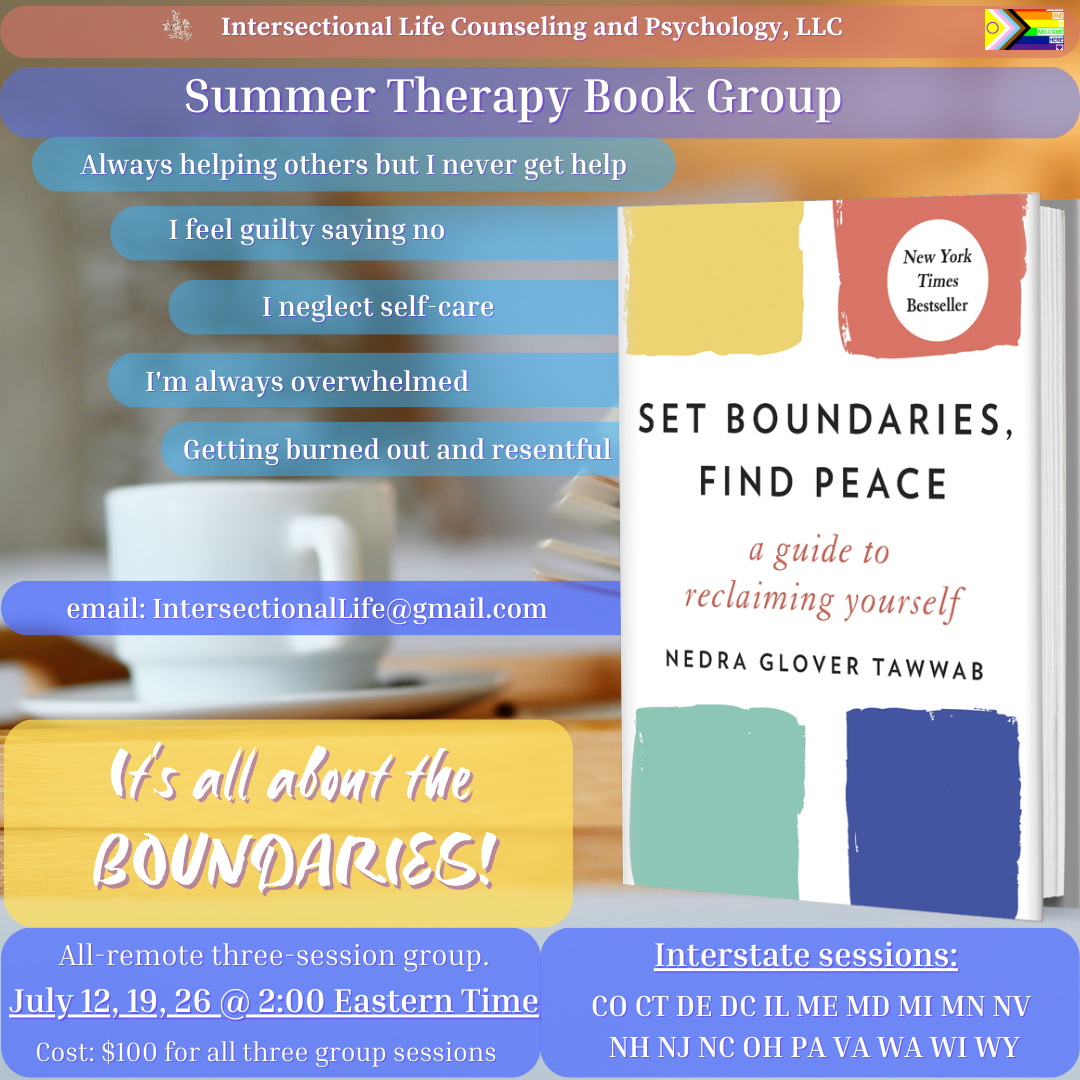
We offer remote therapy sessions anywhere within Pennsylvania. Most people qualify for a sliding-scale discount; use the calculator to instantly see what your fee would be. Email IntersectionalLife@gmail.com to schedule a session.